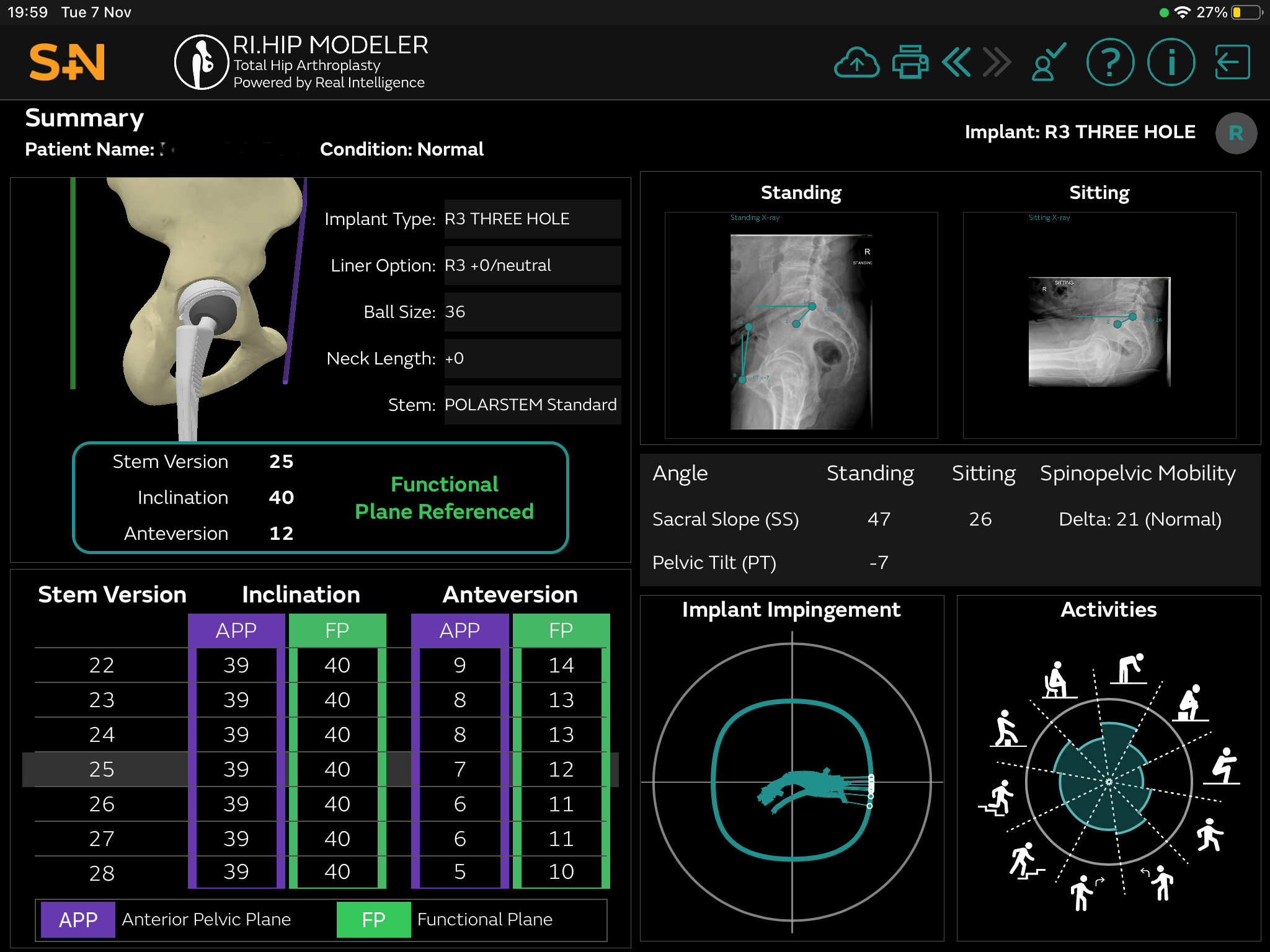
Pre-operation planning screen. Implant optimal position for best range of movement to suit the patient.
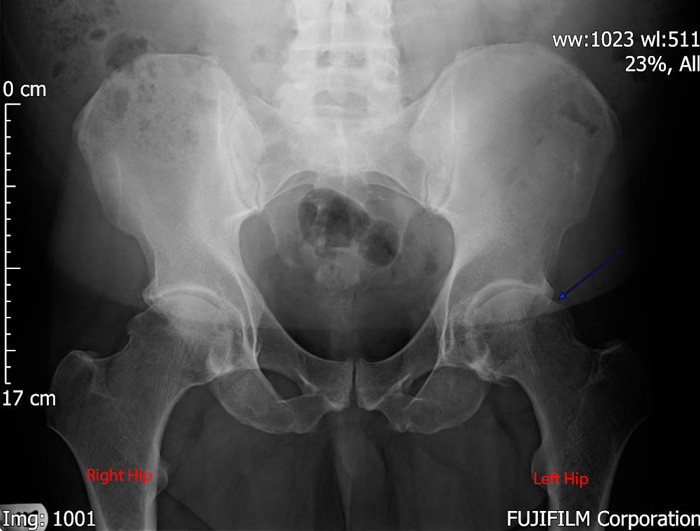
X-ray of the pelvis showing both hips have arthritis. The space between the ball and socket is reduced on the Right. On the Left side the space is not seen (blue arrow) and the bone of the femur (ball) is contacting the bone of the socket.

X-ray of the pelvis after a Left Total Hip Replacement. The Uncemented implant restores the ball and socket joint.
Robotic Total Hip Replacement
Total Hip Replacement
Hip replacement surgery involves removing the damaged joint surfaces (i.e. the worn cartilage and bone), and replacing them with an artificial ball and socket joint.
Due to the engineering advances in recent years, the majority of patients find that after their hip replacement they experience significant pain relief and improvement in movement. This means that they find everyday functions such as sitting, walking and driving much more comfortable.
Results of surgery can be relatively quick but may take between 2 and 6 months depending on the type of surgery you have, your overall health and how well you rehabilitate.
How long the replacement hip lasts can depend on many factors, although it is true to say that most patients will never need to have another operation. The amount of activity you undertake may have a bearing on the life of the joint, as will your weight. Overall a replacement hip might be expected to last fifteen to twenty years.
Robotic Hip Replacement Surgery – improving accuracy
Robotic surgery has improved what we can achieve at the time of a total hip replacement.
The robot allows improved accuracy in measurement and placement of the new joint helping to control leg length and offset, whilst allowing control of socket position to reduce the chance of dislocation and implant impingement.
Using the Real Intelligence software the implant positions are tailored to fit your skeleton through a wide range of movement – paticularly difficult to achieve if there is a significant lower back stiffness from surgery or wear and tear.
I am a member of the Computer Assisted Orthopaedic Surgical Association, which is part of the British Orthopaedic Association.
Improving Outcomes
Faster surgery and recovery.
More accurate implant positioning – more chance of joint lasting longer up to 25 years or more.
Less chance of leg length inequality and dislocation.
If you have a painful hip that’s holding you back, don’t struggle on, get in touch and book an appointment.
Robotic Total Hip Replacement FAQ
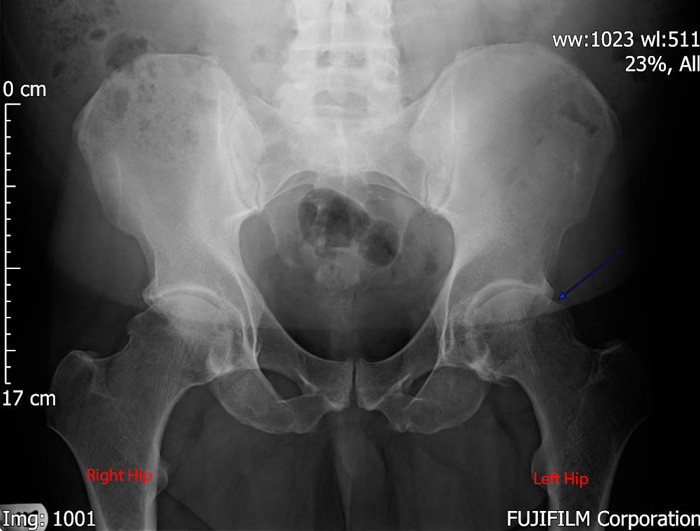
X-ray of the pelvis showing both hips have arthritis. The space between the ball and socket is reduced on the Right. On the Left side the space is not seen (blue arrow) and the bone of the femur (ball) is contacting the bone of the socket.

X-ray of the pelvis after a Left Total Hip Replacement. The Uncemented implant restores the ball and socket joint.
FAQs
Many of my patients tell me that their knee replacement surgery
has been life-changing
has been life-changing
and they’d wished they’d had it done sooner. Patients who do best, are patients that do a little bit of ‘pre-habilitation’ work to strengthen before their surgery, and really embrace the post-op physio rehab making sure they do their daily exercises.