MRI scan of knee showing complete rupture of the ACL at its top end (Red Arrow). White represents inflammation and the dark grey bottom end of the ligament is intact. MRI is useful for showing other injuries.
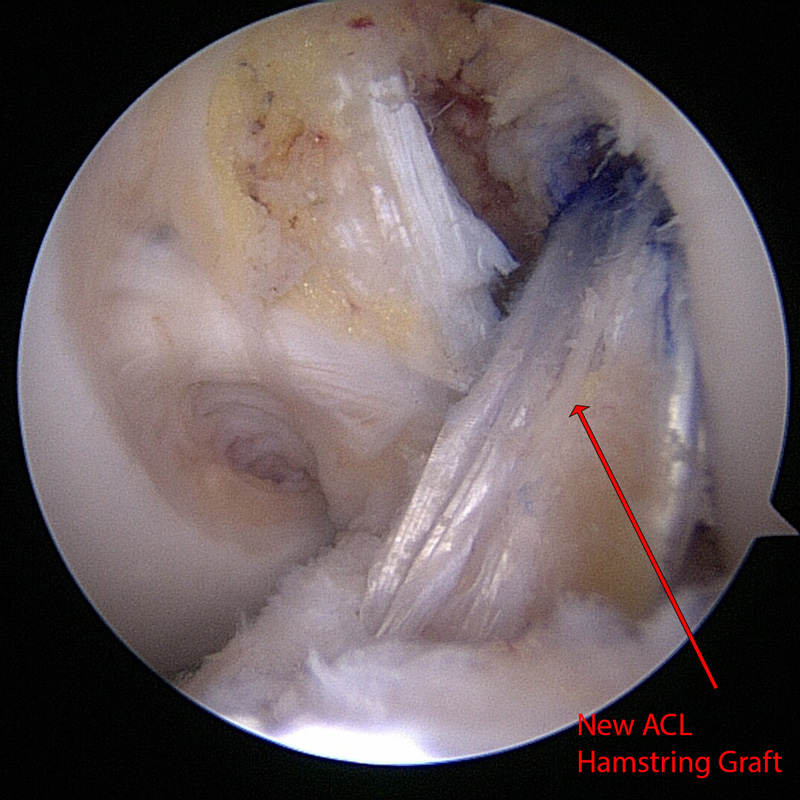
Left Knee ACL reconstruction with multiple strand hamstring graft. The new ligament (Red Arrow) is seen in place of the removed damaged ligament with the knee flexed to 90 degrees.
ACL Recostruction
What is the ACL?
The anterior cruciate ligament is one of 4 major ligaments around the knee. It serves to provide central stability to the joint particularly on twisting and pivoting movements.
How is the ACL injured?
It is often injured during sporting activity but occasionally can be torn with minimal trauma. Usually there is a history of twisting of the knee or change of direction with the knee collapsing. There can be an associated “pop” as the ligament fails.
The injury may be accompanied by tears to the meniscal cartilage, joint surface damage or may be part of a multiple ligament injury.
Swelling usually occurs within hours and there is often the feeling of the knee popping out of joint. It is rare to be able to continue playing sport with the initial injury. Once the initial injury settles down the main symptom is instability or giving away of the knee. This usually occurs with running activities but can occur on simple walking or other activities of daily living.
Diagnosis of ACL injury
The diagnosis is made from the history of the injury and the clinical examination of the knee. This is often aided by investigations such as an X-ray (to rule out fracture) and an MRI scan which gives detailed information about knee structures.
Treatment of ACL injury
Treatment is always directed to suit the patient. Initial management is to treat the acute knee injury (rest, ice, compression and support) and start early muscle rehabilitation. You may see muscle loss only hours after a knee injury.
With simple rehabilitation and physiotherapy the knee may settle down and be perfectly stable when returning to normal activities.
Will surgery be needed?
If the knee is unstable due to the injury then there is the possibility of further damage to other parts of the knee. With simple rehabilitation the knee may improve, but if instability persists then a reconstruction may be required.
Active adult patients involved in sports or jobs that require pivoting, turning or hard-cutting as well as heavy manual work, will tend to require surgical treatment.
Activity and stability, not age, should determine if surgical intervention should be considered.
If you have had a knee injury and are worried about your ligaments please book in to see me for a consultation. I would be delighted to see you and help sort out the problem.

MRI scan of knee showing complete rupture of the ACL at its top end (Red Arrow). White represents inflammation and the dark grey bottom end of the ligament is intact. MRI is useful for showing other injuries.
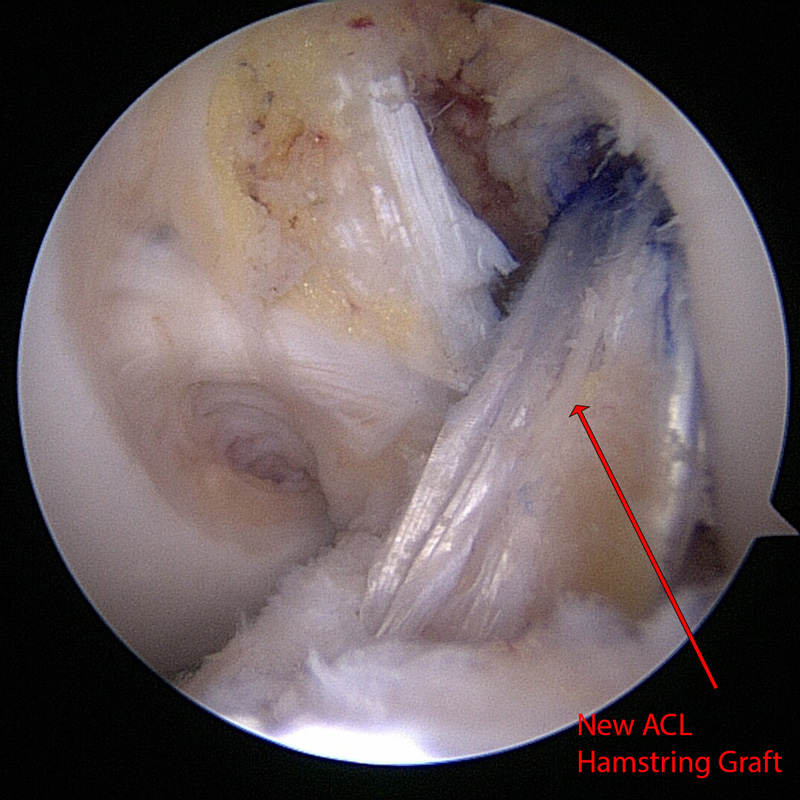
Left Knee ACL reconstruction with multiple strand hamstring graft. The new ligament (Red Arrow) is seen in place of the removed damaged ligament with the knee flexed to 90 degrees.