Please ask questions if you are unsure or need more clarification as it is important that you have enough information to fully weigh up the benefits and risks of surgery.
General risks of surgery include:
- Allergies to anaesthetic agents, antiseptic solutions, suture materials or dressings
- Pain and discomfort around the incisions
- Nausea, typically from the anaesthetic, this usually settles down quickly
- Bleeding from the incisions
- Separation of wound edges
- Slow healing – most likely to occur in smokers and people with diabetes
- Wound infections
- Blood Clots (Deep Vein Thrombosis or DVT, Pulmonary Embolism or PE)
What are the side effects and risks of revision knee replacement surgery?
We define a side effect as an inevitable consequence of the operation but not necessarily of benefit to the patient. The obvious example being the scar which will be about six to eight inches long down the front of the knee. Another inevitable consequence of knee replacement surgery is some degree of numbness around the scar, which may be permanent. Because of this and the site of the scar, people’s ability to kneel after knee replacement varies. About 50% of people find they can manage it with some degree of comfort but it is never as easy as it was before the operation.
Revision knee replacement is a bigger operation than a primary knee replacement, with a number of rare but well recognised risks. In general, the profile of risks and complications for this surgery are similar to those for primary surgery but the incidence is slightly higher.
The most serious and common are outlined below:
Infection:
A serious deep infection occurs in approximately 1% of cases although superficial minor infections around the scar are a little more common but usually do not lead to long term trouble and can normally be managed with antibiotics alone. In deep infection, the joint replacement almost always has to be removed and another one put in some time later. This is called a two-stage revision.
At the first stage the joint replacement is removed, the knee is washed out, and the infection tested so that we know which antibiotics to use. The antibiotics are then given either by mouth or by intravenous drip and treatment might need to continue for at least six weeks, and possibly a lot longer, depending on the type of infection and response to treatment. Treatment is monitored by blood tests which indicate whether or not the infection has been cleared. As soon as there is no evidence of any infection the second stage of the operation is done in which a new joint replacement is put in place.
However, even taking these precautions, the risks of a further infection are significant and the whole process might need to be repeated. The success of a two-stage revision is about 80/20, with a 20% chance of either replacing the joint again or having to treat the infection indefinitely with antibiotics. In exceptional cases, the joint has to be fused and ultimately the whole limb is at risk from ongoing infection if it cannot be treated.
The overall amputation rate after total knee replacement for a complication such as this is about one in one thousand.
Deep vein thrombosis and pulmonary embolus:
Deep vein thrombosis (DVT) is a relatively common complication after major lower limb surgery, particularly total knee replacement. It is caused by the blood clotting in the veins of the leg in the deep muscles and leads to pain and swelling of the leg, normally between ten days and six weeks after surgery but occasionally occurring sooner.
Post-operative calf pain, tenderness and swelling are regarded as a serious risk and it requires immediate investigation and treatment. Normally, this can be done with simple ultrasound scanning and medication. If it occurs at home postoperatively, it needs emergency hospital treatment. It is not a situation to leave to the next clinic appointment.
The risks of deep vein thrombosis are:
- Long term pain and swelling in the leg (the post-phlebitic syndrome) which may last indefinitely or 2. The clot can move from the leg into the lung, leading to pulmonary embolus. In extreme cases this can be a cause of sudden death, but more often gives rise to chest pain and shortness of breath. Patients who develop a pulmonary embolus don’t always get the typical symptoms of calf swelling first (a silent DVT). Because of the severe nature of deep vein thrombosis, we go to significant lengths to reduce its incidence by chemical means with drugs, and with pneumatic calf pumps which are used in the pre and post-operative period. We also aim to get patients mobile as quickly as possible after the operation.
Patients already on blood thinning medication, such as Warfarin, should temporarily stop taking this so that a more reversible form of treatment can be used during surgery. The Warfarin can be restarted a few days after the operation. Unfortunately, despite all precautions, it is not always possible to prevent every clot or pulmonary embolus.
Stiffness:
Stiffness is a well-recognised complication of surgery. Our goal is to achieve at least 0 to 100° of flexion (action of bending), which is well over a right-angle bend and permits most normal activities. Sometimes we fail to achieve this range of movement despite appropriate surgery and physiotherapy.
There are a number of causes for stiffness, the most common of which is that the joint was particularly stiff before surgery which means that movement is more likely to be restricted indefinitely. We hope to achieve 70° to 80° of movement in the first few days after surgery and about 90° by six weeks and if these milestones are not met we would recommend a manipulation under anaesthetic (MUA). This requires a general or spinal anaesthetic; it is not usually particularly painful and can often achieve the desired range of movement in the majority of cases. However, permanent stiffness is a recognised complication and can be the cause of an unsatisfactory result.
Persistent pain:
Persistent pain is a recognised complication occurring in about 5% of patients and in a few cases leads to a disappointing result in the long term. There are many causes of this and, as knee replacement is done for pain relief, it is a complication that we take seriously. If the kneecap was not replaced this may be necessary as a later operation.
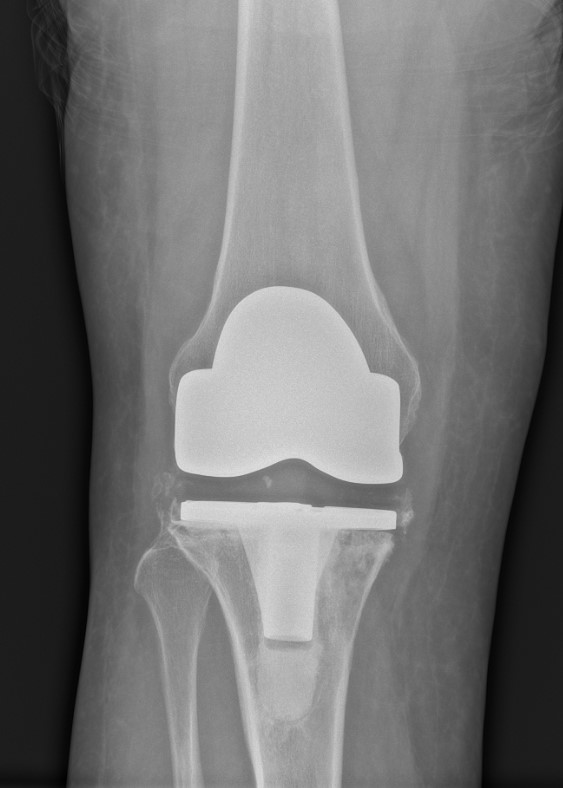
We investigate persistent pain with X-rays, scans and blood tests. Normally we would initially check for infection and then consider loosening the prosthesis on the bone ends. However, in a few individuals, after an apparently successful knee replacement (from a technical point of view), the knee continues to be painful and gives a disappointing result without any easy solution.
Rare and extreme risks
Other rarer complications include fracture at the time of surgery, circulation and/or nerve damage to the foot and lower leg, persistent swelling, instability of the knee and dislocation of the joint replacement.
The overall mortality (risk of dying) is 1 in 300 and is usually caused by a pulmonary embolus or heart attack soon after the operation. The risk of complications leading to amputation of the leg is 1 in 1000.